Pain Management
What is pain?
We all experience pain; some more than others and there are many kinds of pain. There can be sudden pain when we fall and cut our knee or twist our ankle. Pain can be unpredictable – for example, you could lift an object hundreds of times without a problem and then, without warning, one time this same lift causes pain.
Pain can also start with no obvious injury – for example, someone who has worked in an office for 15 years who starts to get neck pain. Pain is how our brain warns us that something might need protecting or is causing damage to our body. We experience pain when our brain processes the information that it is receiving as threatening.
Pain from sprains, cuts and posture are everyday pains. The brain concludes our body tissues are under threat, so we change our posture, or rest our sprained ankle to allow healing and the pain lessens. We remember the uneven ground we tripped on or the posture that caused the pain, our memory helps to protect us from making the same mistake twice.
We have all heard stories of people in the Emergency Department with objects like six-inch nails through their hand. When you look at the nail passing through the damaged tissues you think there must be pain, but when asked they report little or no pain. Tissue damage sends messages to the brain via the nerves, but this does not necessarily result in pain. The ratio of the amount of tissue damage to the amount of pain swings the other way, too.
All of us will have had a paper cut. We know how painful they can be but, at the same time, we struggle to see where the cut is. It can be hard to believe that such a little cut can cause so much pain. This is one of the confusing things about pain. The pain you experience does not relate to the amount of tissue damage. It can be difficult to understand and accept that pain does not always mean harm.
People who live with persistent pain have told us that learning a little more about pain and the nervous system helps them better manage their pain.
The Nervous System
How the Nervous System works?
We have receptors all over our skin. These are nerve endings or danger sensors. Different receptors pick up different information. Some react to temperature; some to pressure. The information that the receptors pick up is sent through the nerves to the spinal cord. The message that is sent is more like a question asking “do I need to protect this?” Not all messages are sent.
We are not aware of every time we are touched. We do not constantly feel our clothes on our skin and sometimes we cannot remember getting the bruise that we discover on our leg. The spinal cord acts like a postal sorting office and decides when and which danger messages are sent to the brain. When enough danger messages reach the spinal cord, the message is sent to the brain.
The brain processes the danger messages and decides if the body is at risk of harm or injury. If the brain decides the body is at risk, we will feel pain and react to get ourselves out of danger. If our hand touches something hot, the danger sensors will send messages to the brain. Our tissues are not designed to withstand much heat, so to protect the hand tissues our brain sends a response of pain and we very quickly remove our hand from the source of heat.
It is sometimes easier to think of how the danger sensors and the brain combine together to form an alarm system. As we mentioned above about the six-inch nail and the paper cut, pain does not always equal harm. Therefore, when we talk about the nerves sending messages, we like to call them danger messages. It is the brain’s use of this information from the alarm system that results in the feeling of pain. The brain is working out “do I need to protect this?”
Most of us will have sprained an ankle at some time in our lives. Remember how quickly after the injury the area became swollen, red and tender to touch? This is because all the chemicals involved in healing arrive at the injury site to do their job and start the healing process. These chemicals irritate the nerves, making the area tender to touch. This reaction has a protective role. The first few days after the sprained ankle you may have rested more or even used crutches to ease the pain when walking which allows the injured tissues time to heal. This type of pain is called acute pain.
Over time, as healing takes place, we can walk easier and, after more time, are able to return to our normal activities. There was a useful reason for this pain. It meant we rested the injury and allowed the tissues time to heal. As the healing takes place, the chemicals stop being produced and the pain should gradually reduce and stop.
This process takes time but the tissues will heal. A broken bone or tendon and ligament injuries will heal within six to 12 weeks. The body will continue to remodel scar tissue for three to six months after healing.
Researchers have learnt more about pain in the past 10 years than in the past 100 years. They can see what changes happen in the nervous system producing persistent pain; even though the tissues are completely healed. For some people the pain starts without damage to the tissues. Unfortunately, we do not fully understand why this persistent pain starts.
This type of pain is called chronic or persistent pain. In persistent pain the brain continues to receive the danger message; it thinks that the tissues may require protecting. The brain decides the body needs all the protection it can get. It starts to adapt and build more defences; it upgrades the alarm system. It needs more information from the tissues, so it creates more danger sensors. The brain thinks, the more information the better!
More danger sensors create more danger signals. All these messages are sent to the spinal cord. The spinal cord or postal sorting office becomes overloaded with messages and starts working overtime to deal with all the extra messages. It becomes quicker at processing the messages and sends out more deliveries, allowing more of the messages to be sent out as soon as they arrive. Before it would have been more selective of which messages needed to be sent. The spinal cord is now starting to amplify the signals it receives from the tissues.
Our brain receives more messages, it becomes better and quicker at recognising the danger messages. The alarm system stays on high alert. This now means that we receive the pain message more often. Levels of pressure and movement that didn’t previously hurt, can now feel painful and things that previously hurt, now hurt even more. The alarm system is now going off, for example, when someone taps the window, instead of only when the window breaks.
The pain starts, it does not go, and you become worried. In the past when you had pain you rested, so now you do the same and avoid movement to protect the area and avoid any potential damage.
The pain stays; you keep the reduced level of activity because any time you try to do more or do something differently, it hurts. Your muscles and tissues become weaker and less flexible as they get used to doing less. When you walk further than normal you may become out of breath and hot. You find that you can no longer do things that you used to find easy. When you become active it takes less to stress your muscles and tissues. When the tissues are stressed they release danger chemicals as the brain is now on alert and quicker at recognising these signals and is more likely to send a pain message.
When tighter tissues, weaker muscles and lots of danger chemicals irritate the over excited alarm system it is not surprising that the smallest stretch starts to feel so painful. Even though the tissues are healed as best they can, you feel pain. This pain can often feel exactly like the pain you had when you initially had your injury. This familiar pain helps to reinforce the thoughts you may be having that there must be something wrong; there must be damage to the tissues. Hopefully, by reading and understanding what has been written so far we know that this is not always true and pain does not always mean harm.
Pain and your memory
Pain memory can be very powerful. Even a memory of a specific situation that caused harm from the past, can elicit the danger alarm system to produce pain and make us act in ways that we think will protect us from further harm; even if there is no real danger the second time round.
Tissue tolerance and pain
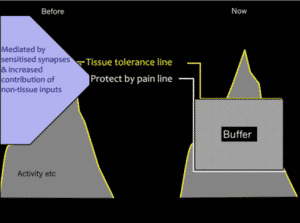
All of our tissues (muscles, ligaments) have a tissue tolerance line – for example, the amount of load the tissues can tolerate before damage occurs. Pain serves as a very clever protection system to the tissues. You can see from the picture below that the point where pain will be generated as a protection is just below the tissue tolerance line. This is useful as it helps to prevent us from injuring ourselves. The pain protection point is triggered by nociceptors (receptor cells producing danger messages) which can be modulated by attention, anxiety, and expectation.
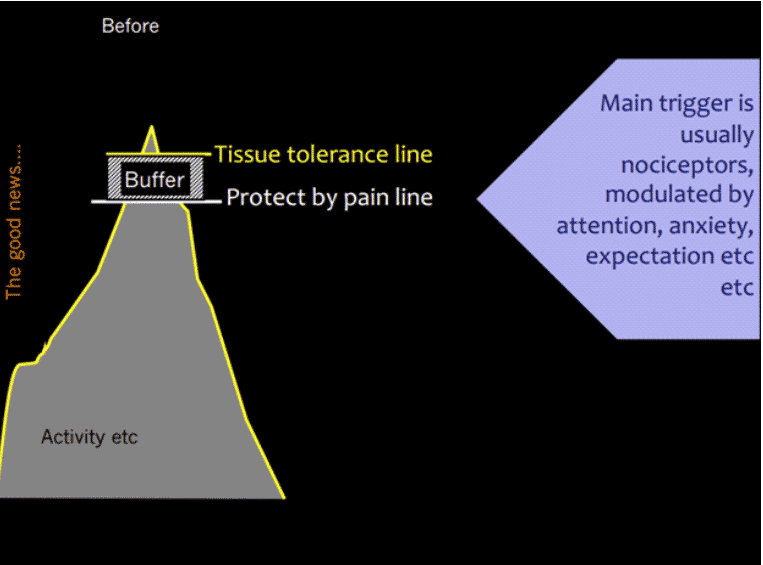
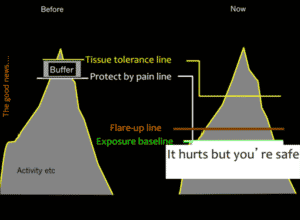
When pain becomes persistent due to the changes in the sensitisation in the nervous system, this system is altered. You would probably agree that your tissue tolerance is lower than before your persistent pain came along? This is not necessarily due to tissue damage, but due to becoming more deconditioned over time through living with pain. The biggest change is in the protect-by-pain line. You can see from the diagram below that this is much lower. This means less activity is taken to activate the pain protection system. The other thing you will notice is there is a much bigger buffer before you reach your tissue tolerance line. This is due to physiological changes in the central nervous system (spinal cord and brain) amplifying the pain protective system.
The good news is that whilst it takes less activity to trigger your pain protective system, it does not mean you are causing damage to the tissues. So the message is, it hurts but you are safe. We recommend establishing your point of flare up and your tipping point or exposure baseline. Working below this point will allow your body to become gradually exposed to the activity, improve your fitness and help to retrain the pain protective system.
Yes, it may be complex but there are things that can be done to help you. The main way forward is to try to retrain the pain system. To do this we need to look at all the things that affect the nervous system and may be contributing to your individual pain experience.
A biopsychosocial experience
Identify your triggers
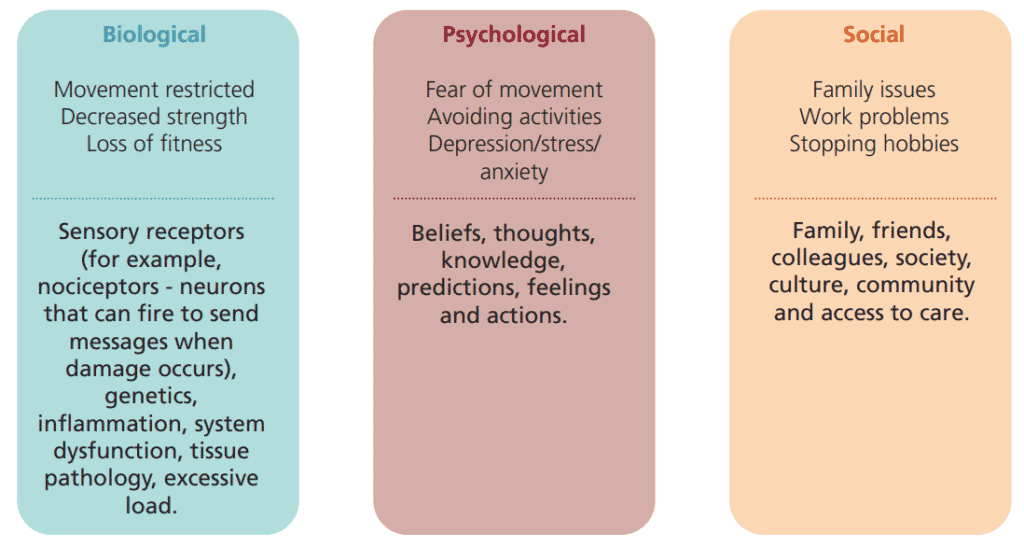
It is essential to look at persistent pain from a broad perspective and considering all of the biopsychosocial factors that can impact on your pain experience. As mentioned before, we know that the brain produces pain when the information that it receives is processed as threatening. This is how all pain is produced – be that acute or persistent, sharp or dull, strong or mild.
What we did not mention before is that the brain receives information from many sources, including biological, psychological, and social information. It is the combination of these bio-psycho-social factors that lead to the brain producing or not producing pain.
Some biopsychosocial factors that contribute to the pain experience include:
When we consider the biopsychosocial perspective of pain, it is easier to understand how we all have a unique experience of pain, and how our own pain can be experienced differently at different times. For example, a soldier fighting in a war zone might sustain an injury with serious tissue damage to a leg, but might not feel any pain until in hospital and away from the danger.
It is likely that the soldier’s brain received information from nociceptors (biological factor), but it probably also received information from the soldier’s belief that “if I stay here I will die” (psychological factor). In this situation, the brain decided it is more helpful to not produce pain in the leg, so that the soldier could run away from the danger prioritising survival. It is important to pay attention to these same biopsychosocial factors when thinking about how to manage persistent pain.
This is an overview of understanding pain. As we talk about pain management strategies, we provide more information about understanding particular aspects of persistent pain in our workshops and information booklets.
It is important to note that this explanation of how pain is produced and maintained applies to all conditions including fibromyalgia, EDS, and osteoarthritis, for example.
Pain does not always mean tissue damage is occurring, and having tissue damage does not guarantee pain will be experienced. Pain comes from the brain and it can be retrained. By looking at your pain experience from a broad/whole person perspective, it gives you lots of opportunities to begin making steps towards retraining your brain.
Self-management
Persistent pain has a considerable impact on the quality of life for many people in the UK. This workbook is an introduction to understanding why we have persistent pain and what we can do about it. Having up-to-date, scientific and usable knowledge about pain is a powerful treatment. You can then use this knowledge to change the things you do, think, say and of course, your level of pain. This can lead to improved function and quality of life.
Many people find that, despite their best efforts and the help they have received from doctors, nurses, physiotherapists, psychologists, their friends and family, they are still left with a substantial degree of pain. They also often find that seeking help and searching for a cure comes with its own problems. People with persistent pain often feel increasingly desperate as time goes on and their pain continues. Each failed new treatment makes this feeling of desperation worse. Sometimes these treatments can produce significant problems of their own, such as side-effects from medicine, discomfort from procedures and exercises that they have tried.
As people live longer, many people will live with a long-term condition. Self-management is crucial for people living with any long-term conditions. On average, people living with health issues spend just four hours per year with their healthcare team; the rest of the time they are managing day-to-day life with that condition on their own. Self-management helps to improve quality of life and put you back in control of your condition.
Self-management encourages you to:
- Find out more about your condition and be more informed
- Learn new skills and tools to help you manage your health and functioning
- Work better, and in partnership, with your healthcare team
- Take charge of your healthcare and choose what is right for you
- Get support from other people in a similar situation to you
Self-management is suitable no matter what your long-term health conditions are – for example, asthma, diabetes, heart disease, arthritis, persistent pain, and anxiety. How people manage their health issues can make a positive difference to their symptoms and functioning.
Health professionals are now involved in enabling patients to understand their conditions, their treatment and self management options. This involves partnership working between the professional and the patient, which is a radically different approach to that of a more traditional medical model perspective.
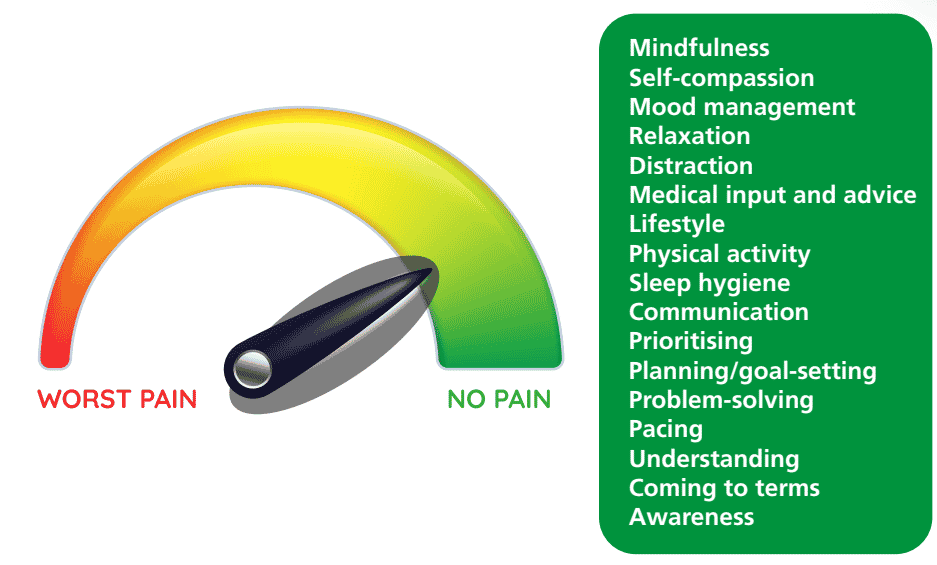
Pain management strategies
Pain management strategies help to enhance self-management and are all research evidenced based. See the dial diagram below for a list of the strategies. These strategies apply to many long-term health conditions such as diabetes, Ehlers-Danlos, fibromyalgia, and rheumatoid arthritis.
Advice on managing pain
- For joint, muscle or generalized pain, you can take non-prescription analgesics such as paracetamol or ibuprofen with food.
- Health care professionals can advise on medications that can help with pain that is not responding to over-the-counter analgesics.
- It can be difficult to completely eliminate persistent pain. Aim to make the pain manageable to allow you to function and sleep better, and to engage in essential daily activities.
- Sleeping well can help reduce pain symptoms. Timing the use of pain medications to coincide with sleep might be helpful if pain is interfering with your sleep.
- Listening to relaxing music or meditation can also help reduce pain levels.
- Pacing daily activities is one of the key tools for managing your pain. Gentle exercise also helps release the body’s internal chemicals, called endorphins, which help reduce pain levels.
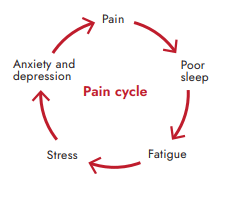
- Be reassured that pain is a common symptom and working through some pain is likely to help break the vicious cycle of pain. You can work through mild pain but don’t exert yourself too much to the extent of worsening pain and fatigue levels (post-exertional malaise (PEM)).
More useful self-management resources
– Understanding pain: https://www.youtube.com/watch?v=C_3phB93rvI
– The scientific power of thought: https://www.youtube.com/watch?v=-v-IMSKOtoE
– Psychological model of pain through metaphors: https://www.youtube.com/watch?v=ZUXPqphwp2U
– Science of pain: https://www.youtube.com/watch?v=ikUzvSph7Z4
– CBT self-help information, resources and tools – https://www.getselfhelp.co.uk/
– Series of podcast episodes about living with persistent pain – http://painconcern.org.uk/airing-pain/
– Listen to ‘Living with Chronic Pain by Neil Berry’ – http://www.paincd.org.uk/
– Healthtalk page about Chronic pain – https://healthtalk.org/chronic-pain/overview
– NHS site with about living with persistant pain – https://www.sheffieldachesandpains.com/persistent/persistent-pain/what-is-persistent-pain/
Resources
Disclaimer: These videos has been created for a Cambridge and Peterborough audience so please ignore any references to the local service, instead use the content appropriately for your own care.
Thank you to the contributors for this section