Nutrition and Hydration
Introduction
Good nutrition and hydration help to support your body in fighting Covid-19 as well as helping to rebuild your muscle strength and function as part of your rehabilitation. Even though you may not feel hungry or thirsty, it is important to eat and drink well.
In the following sections is some general information to help you to maximise your food and fluid intake. If you have specific dietary requirements, please check with a healthcare professional that the information is safe for you to follow.
Nutrition and Hydration management
What you need to do:
Being well hydrated helps your body to function, and aids mobilisation and recovery.
- Drink regularly throughout the day – aim to have eight cups of fluid each day.
- Take small, frequent sips of liquids every few minutes if you are not able to drink large amounts at one time.
- Aim to drink enough fluid to keep your urine a pale straw colour.
- If you have a raised temperature, your fluid needs may be higher.
All fluids (except alcohol) count, try to include nourishing fluids such as milky drinks or juices.

You may require more nutrition than usual to support your body during and after illness.
Dieting with the aim of reducing body weight is not recommended during acute illness or recovery, due to the risk of reducing your muscle mass, strength and ability to carry out day to day tasks.
Long COVID can affect peoples’ appetite and weight in different ways. Some people find they gain unwanted weight and others suffer with a reduced appetite and consequently lose weight.
A well-balanced diet contains foods from all the food groups.
The Eatwell Guide shows how much of what we eat overall should come from each food group to achieve a healthy, balanced diet.
You do not need to achieve this balance with every meal, but try to get the balance right over a day or even a week.
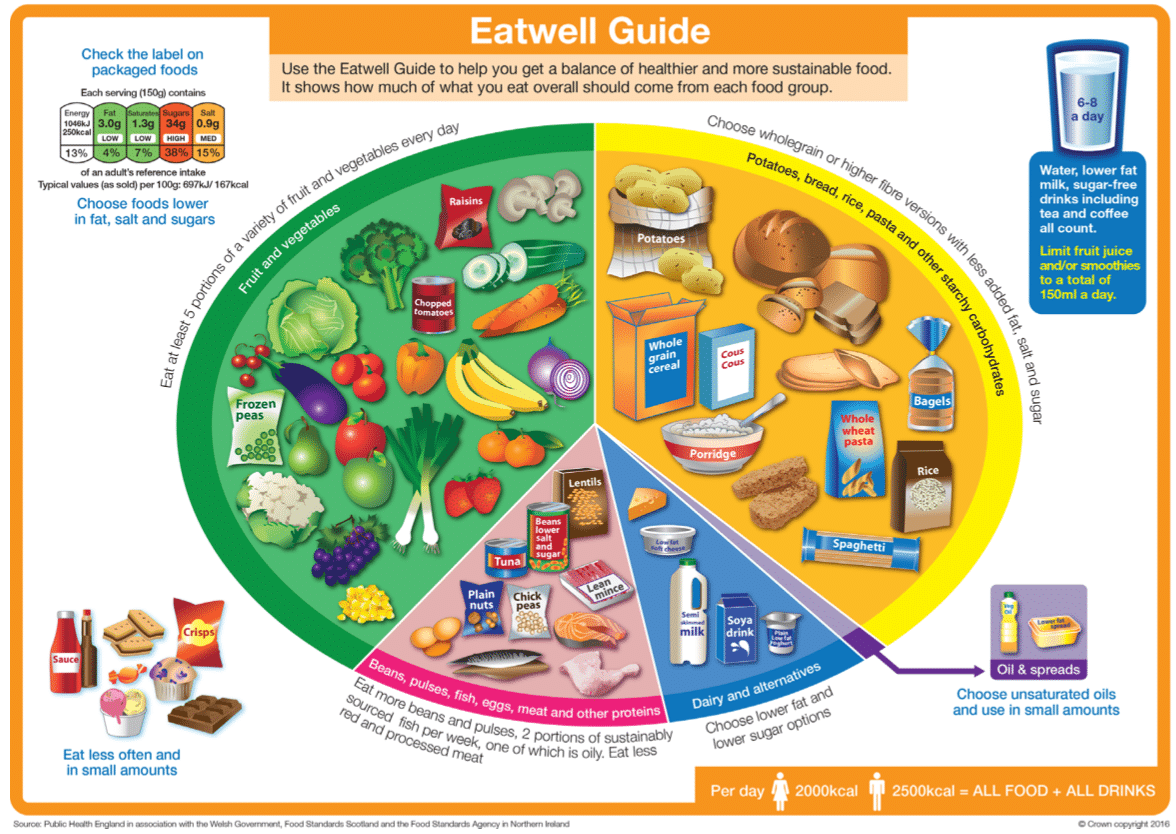
- fruit, vegetables, legumes (such as lentils and beans), nuts and wholegrains (like unprocessed maize, millet, oats, wheat and brown rice);
- eat at least five portions (1 portion = 80 g) of a variety of fruit and vegetables
every day and include vegetables in each meal; - choose wholegrain foods, including wholegrain bread, rice and pasta;
- choose legumes such as beans, lentils and pulses, fish, eggs and lean meat as good sources of protein;
- have some dairy or dairy alternatives (such as soya products) every day;
- limit your intake of salt, fat and sugar:
- salt intake should be less than 5 g per day – about one level teaspoon
- sugar intake should be less than 50 g per day – about 12 level teaspoons
- fat intake should be less than 30% of total energy intake
- choose unsaturated fats found in fish, avocado, nuts and in vegetable oils rather than saturated and transfat; and
- drink plenty of water – aim for 6–8 glasses per day
Some people find themselves eating more than normal due to low mood, boredom, comfort eating or wanting to boost energy levels.
They may also be less physically active and therefore more likely to gain weight.
To help minimise unintentional weight gain keep high fat, sugary foods and sugary drinks to a minimum.
Instead choose healthier alternatives.
For others long COVID can cause a poor appetite which results in eating significantly less than normal.
To help minimise unintentional weight loss eat regularly (by the clock rather than waiting to feel hungry).
Eat little and often having nourishing snacks and drinks in between your meal.
If untreated unintentional weight loss can lead to malnutrition.
Ask your health professional if you are struggling to regain your weight.
- Ensure good oral hygiene with twice-daily toothbrushing.
- Perform smell training, which includes sniffing lemon, rose, clove and eucalyptus for 20 seconds each, twice a day.
- Experiment with herbs and spices like chilli, lemon juice and fresh herbs to add flavour to your foods, but be cautious as these can worsen gastric reflux.
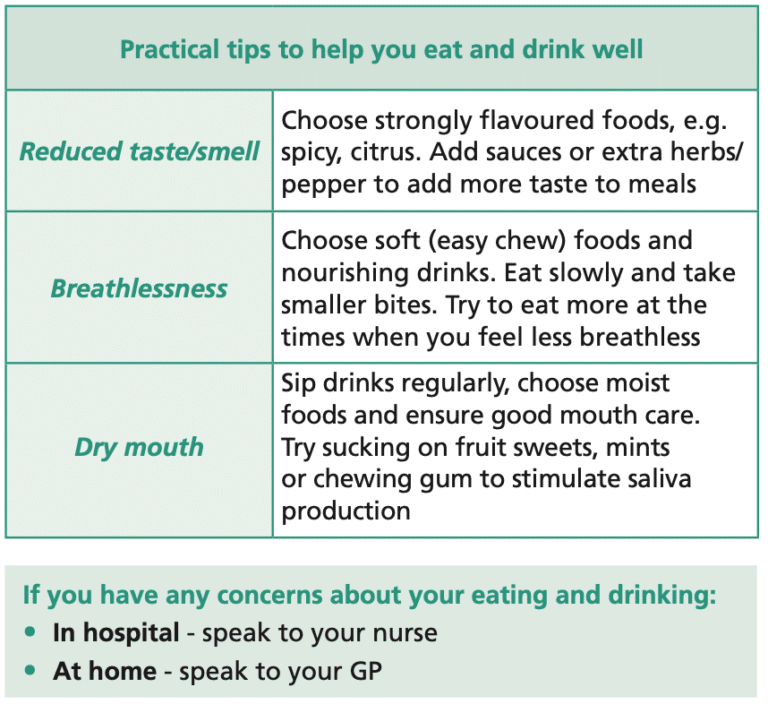
Practical tips to help you eat and drink well
Swallowing advice
How could COVID-19 affect my swallowing?
COVID can affect your breathing. This can interrupt the breathe-swallow pattern as you need to hold your breath momentarily while you swallow. Due to this you may find that you become breathless while eating and drinking or that it is hard to hold your breath to swallow or cough when you swallow.
You may have had a stay in Intensive Care (ICU). This can result in weakening of the muscles used for swallowing as they haven’t been used while you were unwell or asleep. Over time, the muscles will rebuild strength as you build up your intake.
If you had a breathing tube this can sometimes cause some bruising and swelling to your throat and voice box. Sometimes this can result in one or both of the vocal folds not moving properly, which can cause changes to your voice and reduced protection for your airway when you swallow. Usually these affects are temporary and will resolve over time.
Some descriptions of swallowing difficulties:
- Coughing or choking when eating and drinking
- Throat clearing when eating and drinking
- Gurgly/wet voice
- Recurrent chest infections
- Poor appetite
- Weight loss
- Feeling as though food is getting stuck.
- Sit upright whenever you eat or drink. Never eat or drink while lying down.
- Remain upright (seated, standing, walking) for at least 30 minutes after meals.
- Try foods of different consistencies (thick and thin) to see if some foods are easier to swallow than others. It may help to choose soft, smooth and/or moist foods at first, or to chop up solid foods into very small pieces. Take your time while eating and don’t rush.
- Concentrate when you eat or drink. Try to have your meals in a quiet place. Avoid talking while eating or drinking as this may open the airway and cause the food or drink to go down the wrong way.
- Make sure your mouth is clear before taking another bite or sip. If you need to, swallow again.
- Eat smaller meals throughout the day if you get tired when eating full meals.
- If you cough or choke when you eat and drink, seek advice from a health professional, as food or drink may be going down the wrong way into your lungs.
- Keep your mouth clean by brushing your teeth and staying hydrated. If you notice that your tongue is coated or your mouth looks unclean, speak to your GP or pharmacist.
- If you experience any persisting symptoms speak to your GP for a referral to Speech and Language Therapy for further assessment.
Resources
Thank you to the contributors for this section